Your DNA, at least in part, makes you who you are. DNA encodes genes, genes encode proteins, and proteins allow your cells to do their jobs. If anything breaks – if your DNA gets damaged and an essential gene mutates, for instance – the cell can die. Or, often worse, the cell can live, and continue to divide. It can accumulate more mutations, a rolling ball that can culminate in the growth of a tumour. With the risk of cancer in the mix, you might think that cells would pull out all the stops, avoiding any kind of DNA damage at all costs. But increasingly, research is suggesting that DNA damage is just a part of life. Your cells experience tens of thousands of DNA lesions every single day, but for the most part…everything is fine [1].
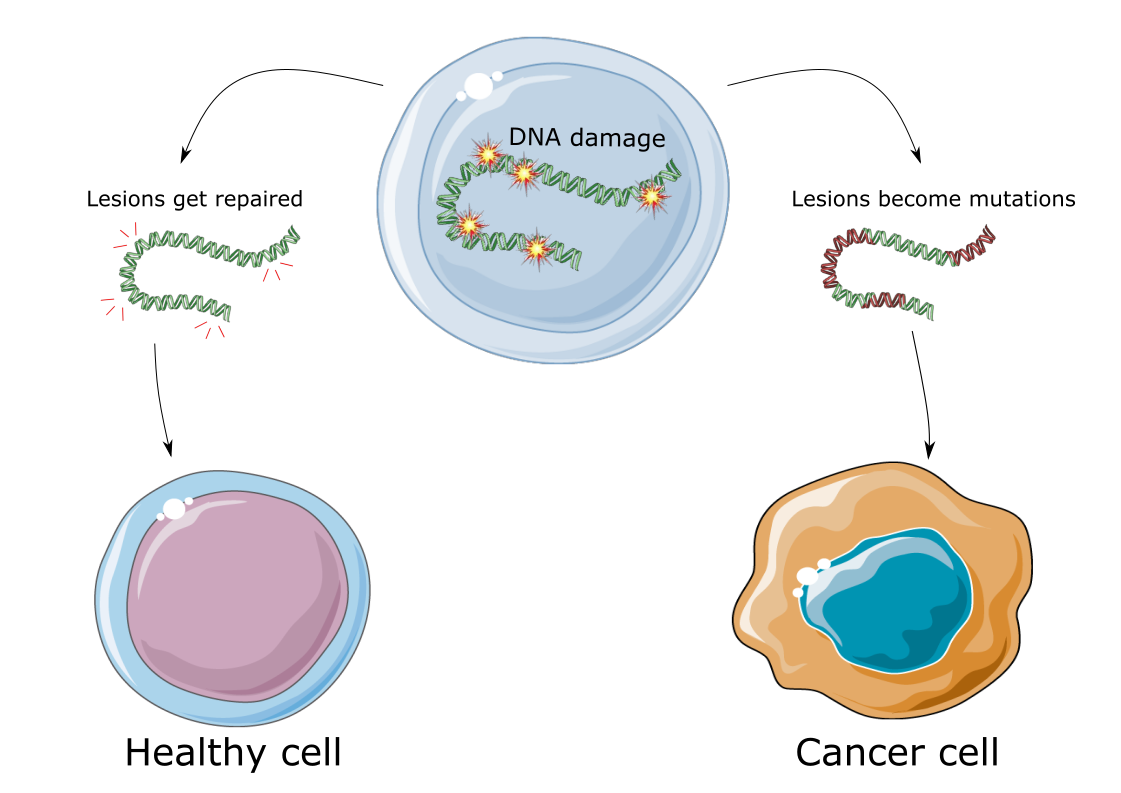
All day every day, each of the specialized cells in your body are executing essential processes that keep you alive and well, like transcribing genes, metabolising molecules into energy, and replicating their DNA to divide into more cells. But as sophisticated as our cells are, nothing they do is 100% perfect, and all of these processes are subject to mistakes. As an example, we can look at DNA polymerase, the enzyme responsible for generating new DNA strands during cell division. It has an error rate of about 1 in 100,000 [2]. In a human cell with 6 billion base pairs to replicate, this enzyme alone would generate 120,000 new mutations with every dividing cell. Similarly, healthy cellular metabolism, like the kind that’s responsible for the citric acid cycle, can generate volatile chemical by-products. These include reactive oxygen species (ROS), which react with DNA bases [3]. A collision with ROS generates DNA lesions (a site of DNA damage, like the base has a bruise) which can then become a DNA mutation (a mistake in the nucleotide code that’s there for good; where we once read an “A” we might now read a “G”) [4]. So, yes, these processes like replication and metabolism are essential to life as we know it. But they come with a side of DNA damage.
And it’s not just about what your cells are doing. As you go about your day, you might expose the cells of your skin to UV light from the sun, ingest alcohol, fly in an airplane where your body is exposed to cosmic rays, or smoke a cigarette. Every one of these activities is known to cause DNA damage, and DNA damage causes mutations [5–8]. To complete the scary story, DNA mutations are the driving force behind cancer. According to an interview with several geneticists and cancer biologists, it’s estimated that your whole body acquires trillions of new mutations every single day [9].
With all that going on, how are we not all walking bags of cancer? There are a few answers to that question, and they’re not mutually exclusive. Several, overlapping cellular systems work very hard to prevent cancer from occurring, despite all the DNA damage that we take on. First, the error-prone enzymes like DNA polymerase have built-in proofreading mechanisms, to catch mistakes before they go too far [10]. Second, DNA lesions, like the ones caused by ROS or UV light exposure, alert the cell’s DNA damage response [1]. The DNA damage response is a huge, cascading set of molecular signals that senses DNA damage, halts the cell cycle, repairs the damage, checks that repair was successful, and releases the cell back into the cell cycle once everything’s okay. If it’s not okay, the DNA damage response can direct the cell to die. (Yes, the DNA damage response does a lot of work). The DNA damage response is what stops most DNA lesions from becoming bona fide mutations, repairing the break before the cell tries to replicate, and if the damage is irreparable, it takes the cell out of the rotation, stopping cancer before it starts.
Thirdly, even if cells do manage to accumulate potentially dangerous mutations, they can sometimes be found out by the immune system. All cells use a molecule called MHC (major histocompatibility complex) to display tiny pieces of the proteins inside them on their surface, for patrolling immune cells to check out. This lets the immune system know whether or not a cell is healthy. If the cell is infected with a virus or bacterium, the cell will start to display viral or bacterial proteins on MHC rather than healthy human cell proteins, and the immune system will know that something is not right. The same process allows a cell to display the results of unrepaired DNA damage: Mutated genes become mutated proteins, and the immune system can see those proteins when they’re presented by MHC [11,12]. If the immune system finds a damaged cell displaying mutated proteins, it kills it, nipping a potential cancer in the bud.
A final major reason why all of these mutations do not cause each of us to sprout uncontrollable cancers every day of our lives is this: One mutation isn’t enough. In a study published earlier this year, researchers looked at the sequenced genome of thousands of cancers and their matching normal tissues, for example a breast cancer compared to a normal breast biopsy. Specifically, they looked at 2,658 whole-cancer genomes, across 38 different types of tumours. They found that, on average, cancers contained twenty thousand mutations compared to their matched normal tissue…but only five of those mutations were actually responsible for the cancer’s progression [13]. These five are called “driver” mutations, and the other twenty thousand are “passengers”. This means that for a burgeoning cancer to even have a leg to stand on, you would need to accumulate just the right (or just the wrong) five mutations, all in the same cell – but there are thousands of other spots where carrying a mutation probably won’t put you in danger.
The importance of your cell repairing DNA lesions before they become DNA mutations can’t be understated. If a lesion isn’t repaired, and a cell goes through mitosis to deliver that lesion to both of its daughter cells, the lesion can collapse into a different mutation in each of those cells. If the cell goes through four or five rounds of cell division with unrepaired lesions, the potential combinations of mutations at that damaged site only go up, increasing the likelihood that you’ll hit upon a mutation that outs you at risk for cancer [4]. That’s where your DNA damage response protects you, by stopping cell division until the lesions are repaired. With all of these safeguards in place, chances are you can live a normal life, DNA damage and all, without having to worry about cancer anytime soon. But if you can reduce your damage risk, for example by avoiding well-known toxic agents like the tar in cigarette smoke, your DNA damage response will thank you for it.