Here is a terrifying statistic: Cancer is one of the top leading causes of death, globally. To put that into perspective, 1 in 6 deaths around the world is because of cancer (1). By definition, it is a large group of diseases that can start in almost any organ or tissue in the body when cells start to grow uncontrollably (1). The burden that cancer brings to the healthcare system, the community, families, and individuals is massive. Financially, economically, physically, and emotionally, cancer is a constant battle that we continue to fight every single day. It is a battle where patients, families, healthcare workers, researchers, and many more come together with the hopes of a common outcome: to cure it.
What is tumour heterogeneity?
However, curing cancer is not as easy as it sounds. Cancer research has been ongoing since the 1700s, and we are still reaching huge milestones of discoveries to this day (2). I’ve seen many posts online throughout the years that say “the cure for cancer has been found, but it’s being withheld from the public” or variations thereof. Although it is optimistic to think that the cure for cancer as a whole has already been identified, it is worth emphasizing that cancer is a large group of diseases. Each cancer type behaves differently from one other, and even cancers of the same organ or tissue can behave differently from one another. This difference is defined as tumour heterogeneity. Tumour heterogeneity essentially states that tumour cells can show distinct morphological and phenotypic profiles, such as differences in gene expression, motility, and ability to spread. More specifically, we have intertumoural heterogeneity, which observes profile differences between tumours, and intratumoural heterogeneity, which observes profile differences within a tumour. Therefore, there is no “one-size-fits-all” therapeutic intervention that can blanket this large group of diseases we call cancer, especially if there is so much heterogeneity.
What is metastasis?
To make things even more complicated, cancer becomes deadlier when it spreads to different organs/tissues in the body, which is called metastasis. The primary cause of death in most cancers involves metastasis. For cancer cells to successfully form metastatic tumours in different parts of the body, they must complete what is called the metastatic cascade (Figure 1).
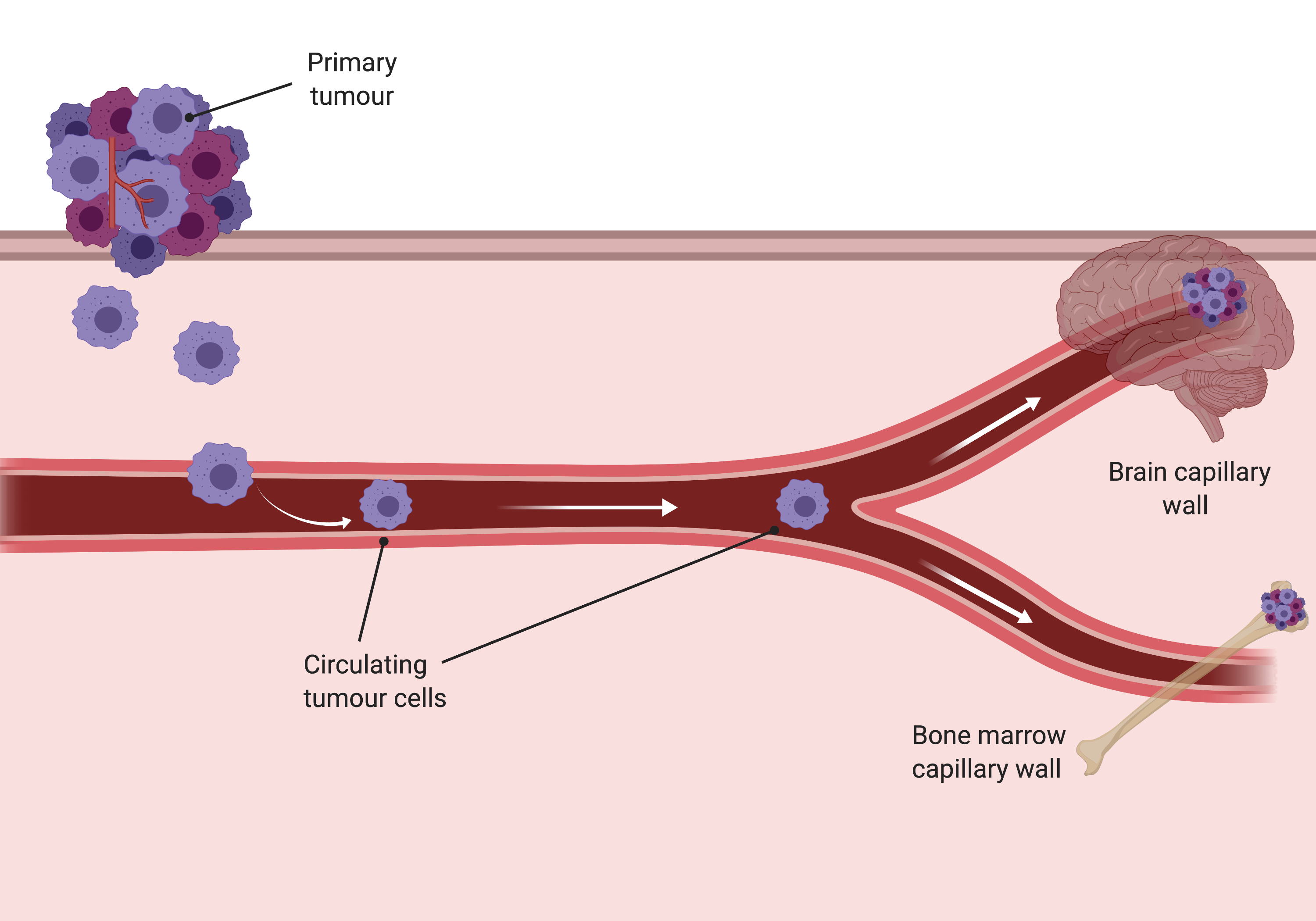
Malignant tumours start early on the road to metastasis. The primary tumour can shed millions of cancer cells within a timeframe of minutes to hours, and these cells can enter the circulation and travel to capillary beds in distant organ sites, such as the brain or bone pictured above (3).
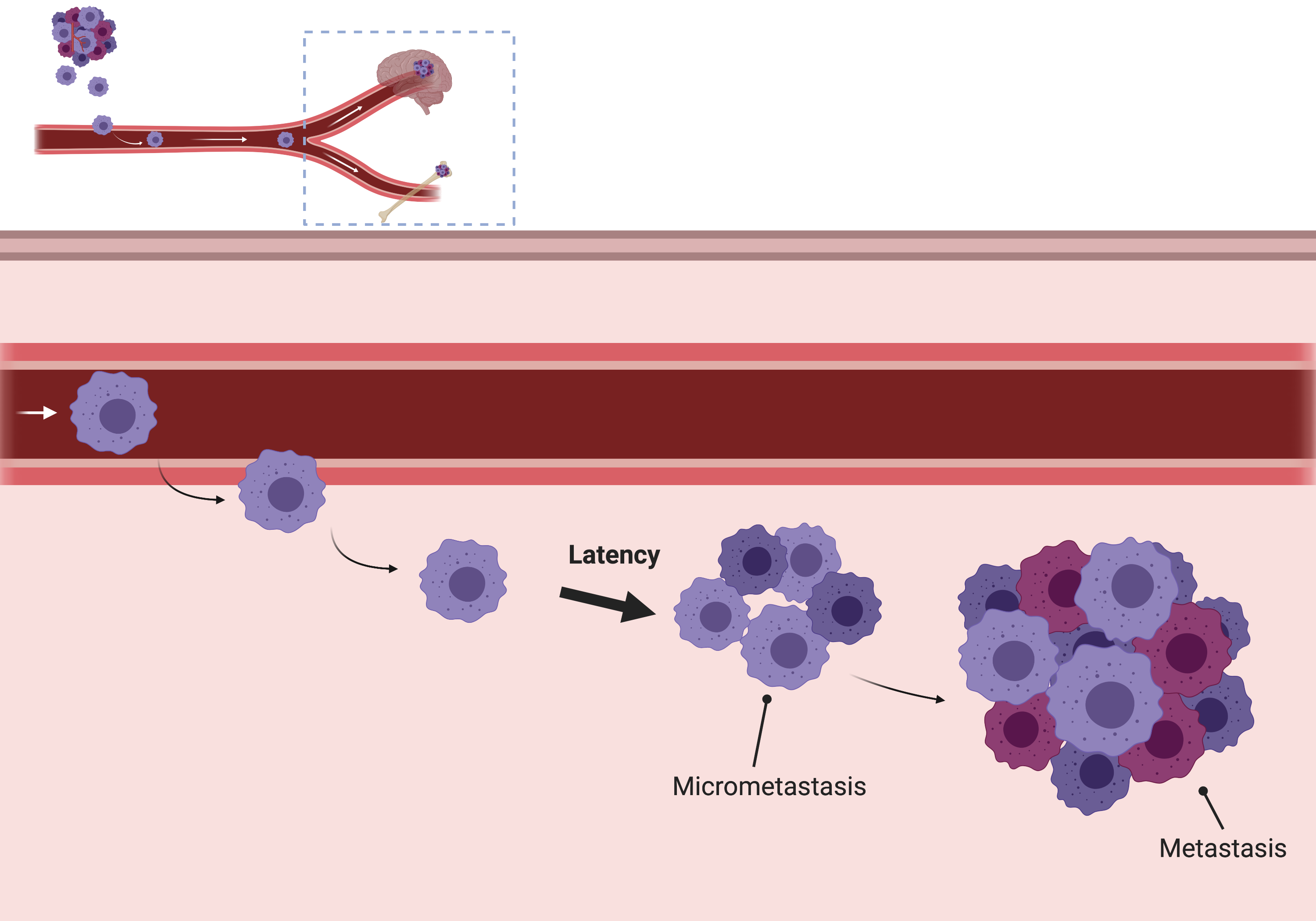
Then, once these tumour cells survived the circulation and reach these distant organ sites, they will enter the surrounding tissues and enter a phase of latency. Tumour cells enter this latent phase, which can range from months to decades. This is a huge factor of how fast cancer can spread, and this is why sometimes we see patients relapse months later vs. patients that relapse decades after treatment (3). The length of latency depends on the oncogenic status of the tumour cells, their ability to proliferate, and the surrounding microenvironment (4). If a patient has a weak host immune response, weak tissue responses, and a particularly advanced stage cancer, the latent phase can be much shorter compared to patients with stronger defense systems and an early stage cancer. And even then, there can still be variability. Metastasis is actually considered to be a very inefficient process – less than 0.01% of tumour cells ultimately form metastatic lesions, and this could also be an understatement as the metastatic cascade is often very tough for cancer cells to successfully complete. So sometimes, there are patients that won’t have metastatic tumours because many of their tumour cells had troubles successfully completing this cascade, especially surviving the lethal signals of the immune response and host tissue defense mechanisms.
However, for those cells that do survive and break out of latency, they can form micrometastatic lesions, then finally, an overt metastatic lesion. Recent studies have suggested targeting the metastatic latent phase as a new direction of research that could show promise in eliminating metastatic seeds prior to their development into these aggressive and often fatal metastatic tumours (4).
So, how fast does cancer spread? Simply put, it varies. It varies from organ to organ, patient to patient, between cancer types, and so on. Cancer is such a deadly disease because of all this variability. Due to advances in medical technology and research, we are working to find more specific targeted therapeutic options for not only the wide variety of cancer types and the wide range of its severity, but also its ability to spread to different parts of the body. As metastatic cancer is responsible for most of cancer-related deaths, it is hopeful that these new advances can shed light into identifying novel therapies that can target the spread of these tumour cells.